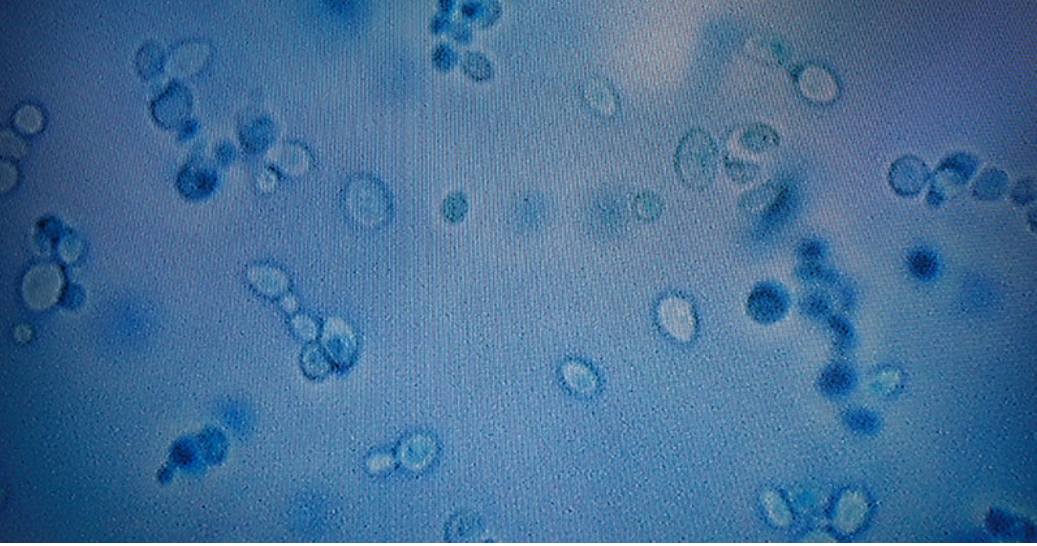
The COVID-19 virus has dominated the national media for years, but in its wake, another deadly disease has gained traction in the United States that has not received nearly as much coverage. Candida auris—a fungal infection that, according to the Center for Disease Control and Prevention (CDC), spread at an “alarming rate” during the coronavirus pandemic—has continued to increase in number of cases during the past few months. It is particularly dangerous due to its resistance to treatment of common antifungal medications. The CDC reported in 2019 that 30% to 60% of people who contracted Candida auris infections have died.
According to Vice President of the American Medical Association Andrea Garcia, over the course of 2021, state and local health departments around the country reported 1,474 clinical cases, about a 200% increase from the nearly 500 cases in 2019. As of 2023, the fungus has been tracked in 28 states and is on the rise nationally. Florida is the state with the third-highest number of cases with 349 infections.
As to why cases have begun to rise, “many factors influence how populations spread, including populations of pathogens,” Associate Professor of Biology and Environmental Studies Brad Oberle explained.
“Increased prevalence could simply reflect more time, changes in the pathogen due to evolution, changes in the host behavior that increases transmission or improvements in public health surveillance and detection,” Oberle elaborated.
It is likely that the coronavirus pandemic worsened the spread of the fungus, CDC officials have said. With attention focused on COVID-19, less emphasis was put on screening for Candida auris. The fungus also tends to cling to nursing gowns, gloves and other personal protective gear that ideally would be changed frequently, but were reused during the pandemic because of supply shortages. Candida auris can also attach to ventilators or other medical equipment.
The fungus is not a particular threat to young healthy people whose immune systems can fight it off, but it can be transported on skin and clothing. Candida auris preys primarily on the elderly with weakened immune systems, especially those in hospitals with medical equipment attached to them. Those who contract it can experience typical infection symptoms, like fever and chills that can intensify in absence of treatment.
Candida auris is becoming increasingly more dangerous because a growing portion of infections recorded by the CDC are drug resistant and cannot be cured with common antifungal medicines. According to a 2021 report from the Antimicrobial Resistance Laboratory Network, out of 22 clinical and screening cases of the infection that were conducted in Texas, seven were found to be resistant to a frontline treatment class of drugs called echinocandins. If resistance to echinocandins becomes more common as the germ evolves, the fungus could become extremely difficult to treat, if not impossible given the limited number of classes of antifungals currently available.
“Viruses have no cells to protect them and are the easiest to destroy,” Oberle explained in regards to disinfecting for fungi. “Bacteria vary in their protection, from zero to two or more cell walls, which makes certain kinds more resistant than others. All fungi have one cell wall that helps protect them. Still, concentrated bleach or ethanol is usually enough to kill them.”
CDC laboratory evidence suggests that “high levels of chlorhexidine are active against Candida auris. However, the effects of chlorhexidine on reducing C. auris skin burden or infection have not been systematically assessed. Outbreaks and transmission have been observed in facilities routinely using chlorhexidine bathing.”
In 2018, out of 51 cases, 23 patients infected with Candida auris died within 90 days. However, it’s difficult to get a sense of how many deaths to attribute directly to the fungus. The reason is that people who become infected are also typically dealing with multiple other health challenges, so Candida auris can be both a cause of death or something that, along with other poor-health factors, hastens it.
New York and Illinois’ intensive efforts to stop the spread of the fungus in health care systems seem to be mostly effective. Candida auris was first detected in significant numbers in those states, and the biggest defense is being able to detect the fungus before it can continue to spread.
“Our best tool to address emerging public health threats is being able to identify them before they begin to rapidly spread,” New York Governor Kathy Hochul stated. “While the CDC report on this drug-resistant fungus is concerning, our ability to track these infections is nation-leading and continues to help us take the aggressive action needed to contain this threat and ensure our health care facilities are safe.”
The Department of Health recommends that when the fungus is confirmed or suspected, patients should be housed in a private room or moved to an area with other patients or residents with the same infection. Hand hygiene and environmental cleaning and disinfection is also critical for preventing the spread of the fungus.